24/7 Medical Billing Services: Streamline Your Revenue Cycle Around the Clock
24/7 Medical Billing Services provide healthcare providers with round-the-clock management of billing, coding, claims submission, and payment follow-ups. By leveraging specialized teams and advanced software, these services improve cash flow, reduce errors, and ensure timely reimbursements, allowing medical practices to focus on patient care while maintaining financial efficiency.
What Are 24/7 Medical Billing Services?
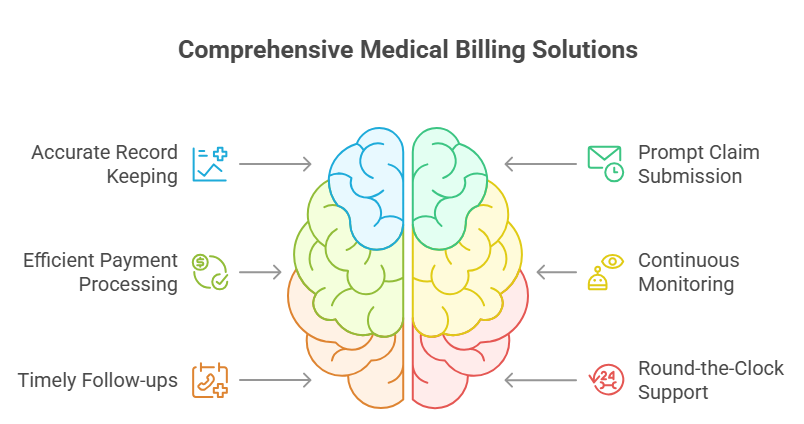
24/7 Medical Billing Services are professional outsourcing solutions that handle all aspects of medical billing and coding at any time of day. These services ensure that healthcare providers, clinics, and hospitals maintain accurate records, submit insurance claims promptly, and receive payments efficiently.
Unlike traditional billing handled in-office during business hours, 24/7 services guarantee continuous monitoring, timely follow-ups, and round-the-clock support. This is particularly beneficial for practices with high patient volumes, complex claims, or multiple locations.
How 24/7 Medical Billing Services Work
24/7 medical billing services operate by handling patient billing, coding, and claims submission around the clock. Dedicated teams ensure that no revenue opportunity is missed, even outside standard office hours. Continuous processing reduces claim backlogs and speeds up reimbursements. This approach keeps providers focused on patient care while experts manage financial operations.
1. Patient Data Collection and Verification
Medical billing begins with gathering patient demographics, insurance information, and medical records. Specialists carefully verify eligibility to prevent errors and claim denials. This ensures that all details align with payer requirements before billing begins. Accurate data collection builds the foundation for smooth revenue cycle management.
2. Coding and Charge Entry
Certified coders assign CPT, ICD-10, and HCPCS codes to diagnoses, procedures, and treatments. Correct coding ensures compliance with industry regulations and reduces reimbursement risks. Charge entry involves mapping these codes to the services rendered for billing accuracy. This step is vital for maximizing reimbursements and avoiding audit issues.
3. Claims Submission and Tracking
After coding, claims are prepared and submitted electronically to insurance carriers, and advanced billing systems track them in real time, flagging denials or rejections. This is crucial because nearly 20% of all claims submitted to HealthCare.gov plans in 2023 were denied, including 19% of in-network claims. Private payers also initially deny about 15% of claims, though more than half are eventually paid after follow-ups or appeals. Continuous monitoring and immediate resolution of issues are therefore essential to improve acceptance rates and maintain smoother cash flow.
4. Payment Posting and Reconciliation
Once payments arrive from insurance companies or patients, they are accurately posted into the system. Any underpayments, discrepancies, or pending balances are quickly identified. Reconciliation ensures the provider’s financial records remain accurate and transparent. This step keeps practices updated on true revenue performance at all times.
5. Reporting and Analytics
24/7 medical billing services deliver detailed performance reports on claims, collections, and outstanding balances. Providers gain valuable insights into revenue cycle efficiency and areas for improvement. Analytics highlight denial trends, patient payment patterns, and financial bottlenecks. This data-driven approach helps healthcare organizations make better business decisions.
Key Features of 24/7 Medical Billing Services
These services include real-time claim submission, denial management, payment posting, and compliance with healthcare regulations. Automated tools help minimize errors while ensuring HIPAA compliance and data security. Round-the-clock availability guarantees smooth cash flow for healthcare providers. Together, these features make billing efficient, accurate, and dependable.
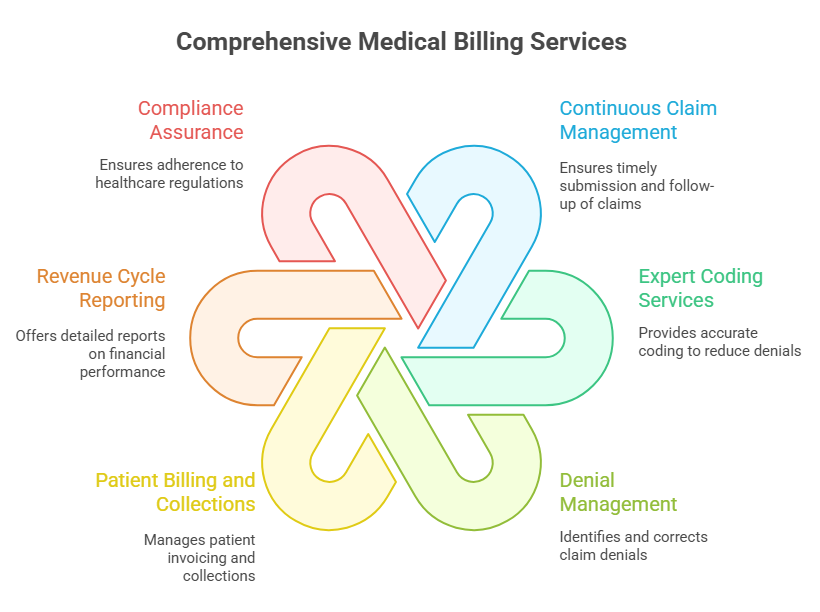
1. Continuous Claim Management
24/7 billing services guarantee timely submission and follow-up of all claims to insurers. Real-time tracking reduces bottlenecks and ensures rejections are addressed immediately. This continuous process minimizes delays in payment collection for providers. As a result, healthcare organizations maintain steady and predictable cash flow.
2. Expert Coding Services
Certified medical coders ensure accuracy in CPT, ICD-10, and HCPCS coding. Proper coding reduces the risk of denials and underpayments from insurance carriers. It also ensures compliance with payer guidelines and healthcare standards. High-quality coding directly translates into maximum reimbursements and reduced audit risks.
3. Denial Management
When claims are denied, billing experts quickly identify the reasons and correct them. They refile claims promptly to recover lost revenue for providers. By analyzing patterns, they can prevent recurring denials in the future. This proactive approach safeguards revenue and strengthens financial outcomes.
4. Patient Billing and Collections
Billing teams manage patient invoicing, reminders, and follow-ups with professionalism, while automated systems ensure accurate statements and flexible payment options. Timely reminders significantly reduce overdue balances, as studies show that practices using automated patient billing systems see up to a 30% improvement in collection rates. This patient-friendly approach not only improves revenue but also enhances patient satisfaction by providing clear, transparent, and manageable billing processes.
5. Revenue Cycle Reporting
Healthcare providers receive detailed, real-time reports on claims, payments, and balances. Analytics highlight bottlenecks in revenue cycles and opportunities for improvement. Transparent reporting improves decision-making and financial planning for practices. Consistent monitoring ensures practices remain financially healthy and prepared for growth.
6. Compliance Assurance
All processes follow HIPAA, insurance regulations, and healthcare compliance guidelines. Providers can trust that patient data is secure and handled responsibly. Strict compliance avoids legal risks, penalties, and costly mistakes. This assurance builds long-term credibility and confidence with both payers and patients.
Benefits of Using 24/7 Medical Billing Services
Healthcare providers gain faster reimbursements and reduced claim denials with 24/7 billing support. By outsourcing, practices cut administrative costs while boosting revenue cycle efficiency. Providers also get real-time reporting and transparency into billing performance. Ultimately, this increases financial stability and enhances patient care quality
1. Improved Cash Flow
Continuous claims submission and follow-ups ensure faster reimbursements from insurance companies, helping healthcare providers maintain steady revenue and avoid cash flow interruptions. Automated billing systems have been shown to reduce overhead costs by up to 40% and cut claim processing time by more than 50%, resulting in faster cash flow and improved financial stability for practices. Regular monitoring minimizes payment delays and enhances financial stability. A streamlined process ensures practices can cover expenses and invest in growth.
2. Reduced Administrative Burden
By outsourcing billing tasks, medical staff can shift their focus back to patient care. Administrative complexities like coding, claims, and compliance are handled by experts. This reduces stress on in-house teams while improving efficiency. Ultimately, providers gain more time to strengthen patient relationships.
3. Minimized Errors and Denials
Experienced coders ensure all CPT, ICD-10, and HCPCS codes are applied correctly. Accurate claim submissions lower the risk of denials and revenue losses. Errors are identified and corrected before claims reach insurers. This proactive approach maximizes reimbursements and safeguards financial performance.
4. Scalability
24/7 billing services are designed to manage increasing patient volumes and multiple locations. Providers can easily adapt to seasonal demand spikes without extra resources. This flexibility ensures operations remain uninterrupted and efficient. Practices can expand confidently knowing billing will scale with them.
5. Enhanced Patient Experience
Accurate and transparent billing reduces patient confusion and frustration. Automated reminders and flexible payment options improve overall satisfaction. Patients benefit from timely updates and error-free invoices. A smooth billing process strengthens trust and loyalty toward healthcare providers.
6. Cost-Effective Solution
Outsourcing eliminates the need to hire and train costly in-house billing staff. Providers gain access to expert services and advanced billing software at a fraction of the price. This significantly reduces overhead and operational expenses. The result is high-quality billing at a lower long-term cost.
How to Use 24/7 Medical Billing Services

Providers start by choosing a trusted medical billing company that offers 24/7 operations. Patient data and claim details are securely shared with the billing team for processing. Regular updates, dashboards, and performance reports keep providers informed. This ensures seamless integration with clinical workflows and efficient financial management.
Step 1: Select a Provider
Begin by choosing a trusted 24/7 medical billing service provider with expertise in your specialty. A provider with proven industry experience ensures compliance with regulations and efficient claims processing. Research their track record, client testimonials, and technological capabilities before committing. The right partner lays the foundation for smooth financial operations.
Once a provider is selected, grant them access to accurate patient records and insurance details. Sharing practice-specific billing policies ensures consistency in claim handling. This step helps the billing team tailor services to meet your exact requirements. Clear communication at this stage reduces future errors and delays.
Step 3: Integration with Your System
Integrate the billing provider’s software with your EMR/EHR system for seamless operations. Proper integration streamlines claim submissions, coding accuracy, and payment posting. It eliminates duplicate data entry while ensuring real-time updates on patient accounts. This step ensures both systems work together to support a smooth revenue cycle.
Step 4: Continuous Monitoring
The billing team actively manages claims, denials, and payments around the clock. Issues are identified and resolved in real time to avoid revenue loss. Continuous monitoring ensures your cash flow remains steady without interruptions. This proactive approach helps prevent backlogs and accelerates reimbursements.
Step 5: Review Reports
Regularly review financial reports provided by the billing team to track revenue cycle performance. Reports highlight outstanding claims, denial rates, and patient balances. These insights allow providers to identify weaknesses and optimize operations. Consistent reporting ensures informed decision-making for long-term financial health.
Limitations of 24/7 Medical Billing Services
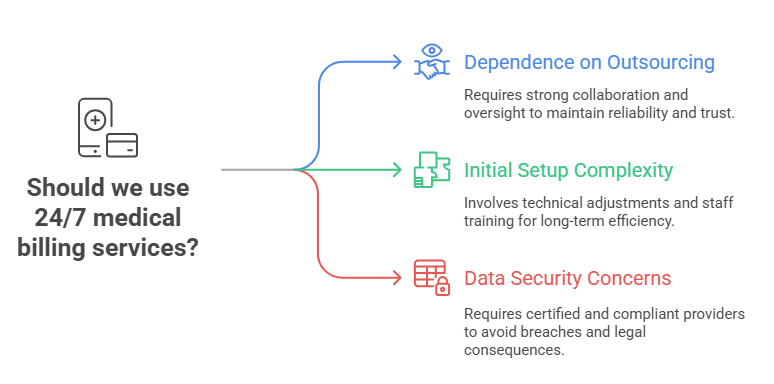
Despite advantages, outsourcing billing means reduced direct control over processes. Time zone differences may cause occasional communication delays with offshore teams. Providers also depend heavily on vendor quality for timely and accurate results. Choosing the wrong partner can impact compliance, revenue, and patient satisfaction.
1. Dependence on Outsourcing
When healthcare providers outsource billing, they rely heavily on external teams for accuracy and efficiency. Any lapse in communication or delays from the provider can affect cash flow. This dependency requires establishing clear service-level agreements and consistent oversight. Strong collaboration is essential to maintain reliability and trust
2. Initial Setup Complexity
Integrating a new billing provider with your existing EMR/EHR system can be complex. The process may involve technical adjustments, data migration, and staff training. While the setup can be time-consuming, it is crucial for long-term efficiency. A structured onboarding plan helps smooth the transition and reduces disruptions.
3. Data Security Concerns
Medical billing involves handling highly sensitive patient information that must remain confidential. Providers are required to follow strict HIPAA regulations to safeguard data. Any breach can result in financial penalties, reputational damage, and legal consequences. Therefore, working only with certified and compliant providers is critical.
TaskVirtual: Your Partner in 24/7 Medical Billing Services
Managing medical billing efficiently around the clock can be overwhelming without the right expertise. Healthcare providers often struggle with claim denials, delayed reimbursements, and administrative burdens that divert their attention away from patient care. TaskVirtual simplifies this by offering end-to-end, 24/7 Medical Billing Services that streamline revenue cycles and maximize financial outcomes.
1. Expert Consultation and Strategy
TaskVirtual’s billing experts assess your practice’s requirements, recommend the best processes, and deliver tailored solutions aligned with compliance standards. From coding accuracy to denial management, their team ensures seamless operations for faster reimbursements.
2. Affordable and Flexible Pricing
Hiring a full in-house billing team can strain healthcare budgets. TaskVirtual provides certified billing professionals at a fraction of the cost, with pricing plans starting as low as $3.12/hour to $14.99/hour, making high-quality billing services accessible to practices of all sizes.
3. Scalable, Accurate Billing Solutions
TaskVirtual ensures error-free coding, claim submissions, and revenue cycle monitoring. Their process emphasizes accuracy, compliance, and scalability—whether handling small practices or multi-location healthcare organizations.
4. Ongoing Support and Real-Time Monitoring
Beyond basic billing, TaskVirtual offers 24/7 support, real-time claim tracking, and proactive denial resolution. This ensures your revenue cycle remains uninterrupted, secure, and optimized—helping providers focus on patient care instead of billing stress.
5. Proven Track Record of Excellence
Trusted by healthcare professionals worldwide, TaskVirtual boasts 364 positive reviews and a 4.7-star rating on leading VA platforms. Their experience in handling complex billing processes allows medical practices to boost efficiency while ensuring consistent financial results.
Conclusion
24/7 Medical Billing Services are essential for healthcare providers looking to improve cash flow, reduce errors, and free up staff time for patient care. By outsourcing billing tasks to certified experts, medical practices can ensure timely reimbursements, accurate claims, and comprehensive financial reporting. For any healthcare organization aiming to streamline its revenue cycle and maintain operational efficiency, 24/7 medical billing is a smart, cost-effective, and scalable solution.
FAQ: 24/7 Medical Billing Services
1. What are 24/7 Medical Billing Services?
They are outsourcing solutions that handle medical billing, coding, claims, and payment processing around the clock.
2. Who can benefit from these services?
Hospitals, clinics, private practices, and multi-location healthcare providers.
3. Do these services include claims follow-up?
Yes, providers continuously monitor and resolve claim denials, delays, and rejections.
4. Can patient billing be managed, too?
Absolutely. These services handle invoicing, reminders, and collections for patients.
5. Is outsourcing cost-effective compared to in-house billing?
Yes, it reduces staff costs, training, software expenses, and administrative overhead while providing expert billing solutions.